Table of Contents
Antibiotic resistance is a growing crisis that threatens to undermine decades of medical progress. As more bacterial strains become resistant to existing treatments, the need for next-generation antibiotics has never been more urgent. Traditional antibiotics, once hailed as miracle drugs, are rapidly losing their effectiveness, and with few new antibiotics entering the market, healthcare systems worldwide are facing an uphill battle against superbugs. However, recent scientific advancements offer hope. This article explores the latest breakthroughs in the development of next-generation antibiotics, highlighting promising innovations that could change the landscape of infectious disease treatment.
Key Takeaways
- Rising Threat: Antibiotic resistance jeopardizes treatment of common infections.
- Superbugs Growing: MDR bacteria, like MRSA, challenge healthcare systems.
- New Discoveries: Novel antibiotics, adjuvants, and peptides show promise.
- Tech Innovation: Nanotechnology and AI drive smarter antibiotic use.
- Urgent Collaboration: Global efforts are key to sustainable solutions.
The Urgency for Next-Generation Antibiotics
The Global Impact of Antibiotic Resistance
Antibiotic resistance poses a severe threat to public health and the global economy. According to the World Health Organization (WHO), antibiotic-resistant bacteria are responsible for at least 700,000 deaths per year, a figure that could rise to 10 million annually by 2050 if no new treatments are developed. Common bacterial infections, such as pneumonia, tuberculosis, and urinary tract infections, are becoming harder to treat, and surgeries, cancer treatments, and organ transplants are increasingly risky due to the danger of untreatable infections.
Infections caused by multi-drug resistant (MDR) bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA), carbapenem-resistant Enterobacteriaceae (CRE), and vancomycin-resistant Enterococci (VRE), are particularly concerning. These superbugs are resistant to multiple antibiotics, leaving doctors with few options for treatment. The rise of these resistant pathogens has led to longer hospital stays, higher medical costs, and increased mortality.
The Stagnation in Antibiotic Development
Despite the urgent need for new antibiotics, pharmaceutical companies have been slow to develop them. The antibiotic development pipeline has stagnated for several reasons, including the high cost and lengthy timeframes involved in bringing new drugs to market. Antibiotics are typically used for short periods, unlike treatments for chronic conditions, leading to lower financial incentives for drug companies. Furthermore, new antibiotics are often reserved as “last-resort” treatments, limiting their market potential.
However, advances in biotechnology, genomics, and artificial intelligence (AI) are now reinvigorating antibiotic research, leading to the discovery of novel compounds and innovative treatment strategies.
Promising Breakthroughs in Next-Generation Antibiotics
Novel Antibiotic Classes
One of the most significant areas of progress in recent years has been the discovery of entirely new classes of antibiotics. Unlike modifications of existing drugs, these novel antibiotics offer fresh mechanisms of action, which bacteria have not yet encountered, reducing the likelihood of resistance development.
Teixobactin, discovered in 2015, is a standout example. This antibiotic represents a new class that targets bacterial cell wall synthesis in a way that makes it difficult for bacteria to develop resistance. Teixobactin has shown promise in preclinical studies against gram-positive bacteria such as MRSA and Mycobacterium tuberculosis. Importantly, bacteria have not yet developed resistance to teixobactin, offering hope for its long-term efficacy.
Another promising new class of antibiotics is odilorhabdins (ODLs). These antibiotics, discovered in symbiotic bacteria found in soil-dwelling nematodes, work by disrupting bacterial protein synthesis. ODLs have shown potent activity against several drug-resistant pathogens, including Escherichia coli and Klebsiella pneumoniae, both of which are responsible for severe hospital-acquired infections.
Reviving Older Antibiotics with New Approaches
While the search for novel antibiotics continues, scientists are also finding ways to revive older antibiotics by overcoming bacterial resistance. One promising strategy is the development of antibiotic adjuvants, compounds that can be combined with existing antibiotics to restore their effectiveness against resistant bacteria.
For example, β-lactamase inhibitors are used in combination with β-lactam antibiotics, such as penicillin and cephalosporins, to counteract bacterial enzymes (β-lactamases) that destroy these drugs. New generations of β-lactamase inhibitors, like avibactam, have proven effective against a range of resistant bacteria, including CRE and Pseudomonas aeruginosa.
Similarly, researchers are working to modify antibiotics like colistin, an older antibiotic that is often the last line of defense against resistant gram-negative bacteria. Through structural modifications, scientists aim to enhance colistin’s activity while reducing its toxicity, making it a more viable option for treating life-threatening infections.
Antimicrobial Peptides (AMPs)
Antimicrobial peptides (AMPs) represent a promising new frontier in the fight against bacterial infections. These small molecules, naturally produced by the immune systems of many organisms, can kill bacteria by disrupting their cell membranes. Unlike traditional antibiotics, AMPs target a broader range of pathogens and are less likely to induce resistance.
One example is pexiganan, a synthetic AMP derived from the skin secretions of frogs. Pexiganan has shown potent activity against both gram-positive and gram-negative bacteria and is currently being investigated for use in treating diabetic foot ulcers, a common site for antibiotic-resistant infections.
Other AMPs are being developed for use as topical treatments, systemic therapies, or even coatings for medical devices to prevent bacterial biofilm formation. Biofilms are clusters of bacteria that adhere to surfaces and are notoriously difficult to treat with traditional antibiotics, but AMPs may offer a way to combat these infections.
Innovations in Antibiotic Delivery Systems
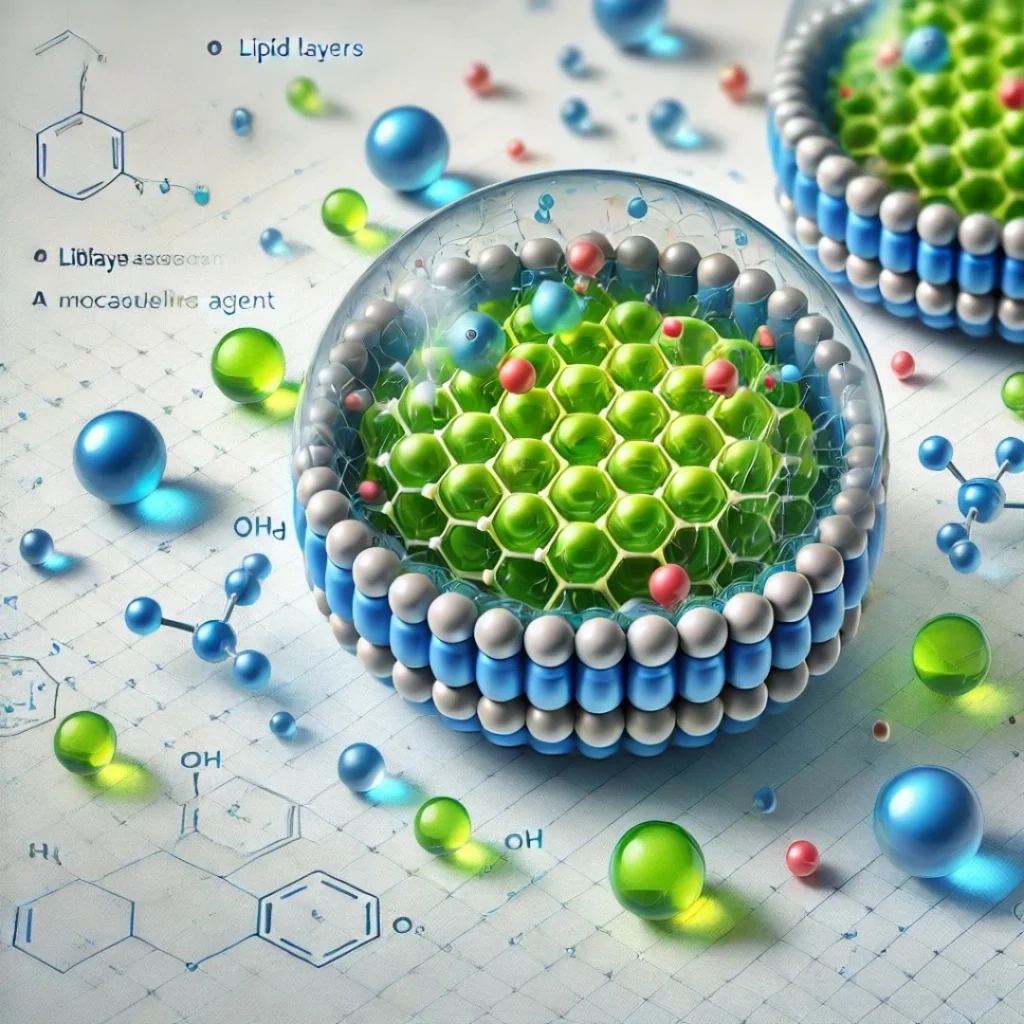
Nanotechnology and Drug Delivery
Nanotechnology is revolutionizing the way antibiotics are delivered to infection sites. Nanoparticles, which range in size from 1 to 100 nanometers, can be engineered to carry antibiotics directly to infected tissues, improving drug concentration where it is needed most and reducing side effects.
Lipid-based nanoparticles, for instance, can encapsulate antibiotics, protecting them from degradation in the body and enabling them to penetrate bacterial biofilms. Biofilms, which are thick layers of bacteria that adhere to surfaces like medical devices, are often resistant to conventional antibiotics. Nanoparticle-based delivery systems can help overcome this barrier by delivering drugs directly to the bacterial cells within the biofilm.
One promising application of nanotechnology is the use of silver nanoparticles, which have intrinsic antibacterial properties and can be combined with antibiotics to enhance their effectiveness. Silver nanoparticles have shown great potential in treating drug-resistant infections by targeting bacterial cell membranes and preventing bacteria from developing resistance.
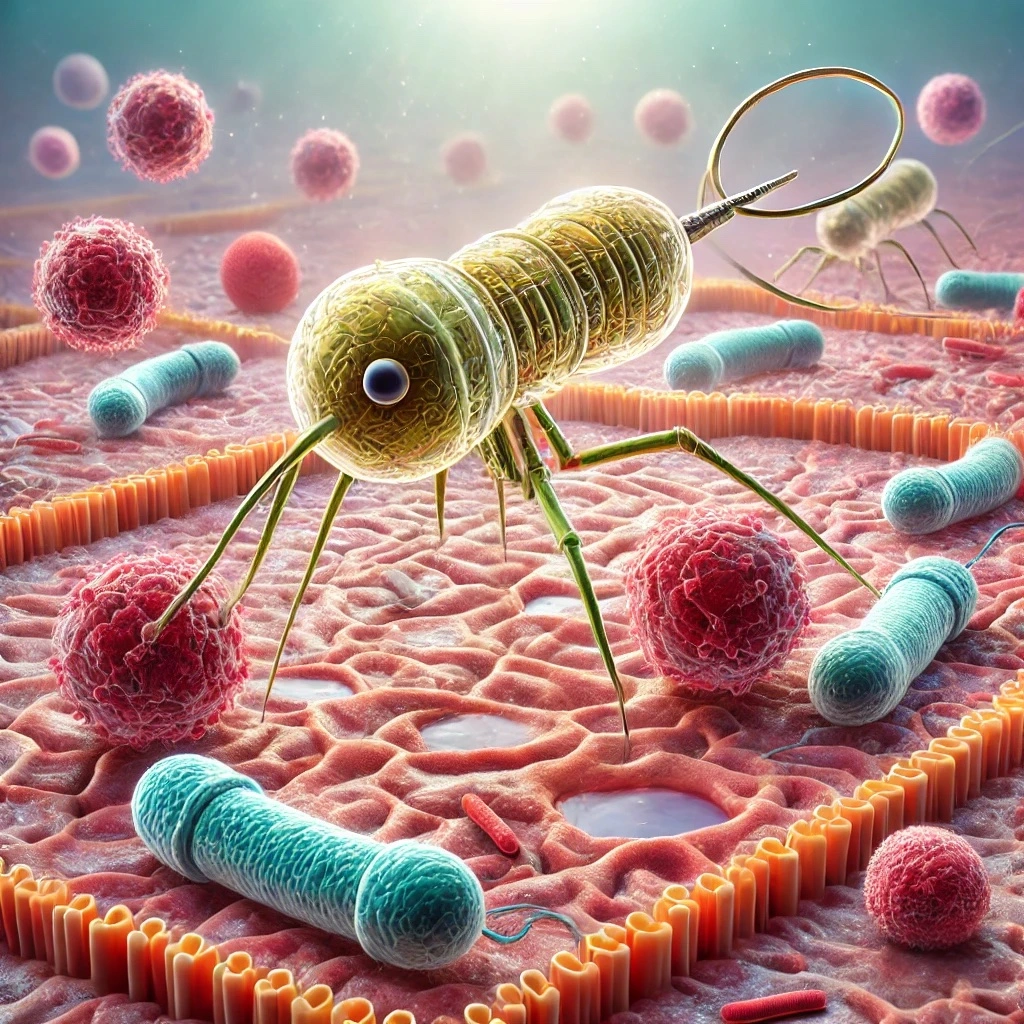
Phage Therapy
Phage therapy, the use of bacteriophages (viruses that infect and kill bacteria), is gaining renewed interest as an alternative or complement to traditional antibiotics. Bacteriophages are highly specific, targeting only the bacteria causing the infection without affecting beneficial bacteria in the body.
Phage therapy offers a personalized approach to treating bacterial infections, as specific phages can be selected based on the strain of bacteria responsible for the infection. This precision reduces the risk of collateral damage to the body’s microbiome, which is a common side effect of broad-spectrum antibiotics.
Recent case studies have demonstrated the potential of phage therapy to successfully treat infections caused by multi-drug resistant bacteria, particularly when conventional antibiotics have failed. Phages are also being used in combination with antibiotics to create synergistic effects, enhancing the overall effectiveness of the treatment.
Artificial Intelligence and Antibiotic Discovery
AI-Driven Drug Discovery
Artificial intelligence (AI) is rapidly transforming the field of antibiotic discovery by enabling scientists to analyze massive datasets and predict the properties of new compounds. Machine learning algorithms can identify patterns in bacterial resistance mechanisms and suggest potential drug candidates that could overcome these defenses.
In one notable success, AI was used to discover halicin, a novel antibiotic effective against Clostridium difficile, Acinetobacter baumannii, and other resistant bacteria. The AI system analyzed over 100 million molecules, identifying halicin as a promising candidate in a fraction of the time it would have taken using traditional methods.
AI is also being used to predict how bacteria will develop resistance to new antibiotics, allowing researchers to design drugs that are less likely to become obsolete due to resistance. This predictive power is revolutionizing the way antibiotics are developed, offering a faster and more cost-effective approach to addressing the antibiotic resistance crisis.
AI-enhanced Combination Therapies
AI is also helping to optimize combination therapies, where multiple drugs are used together to enhance their effectiveness. By analyzing how different antibiotics interact with each other and with bacterial cells, AI can suggest combinations that reduce the likelihood of resistance while improving patient outcomes.
This approach is particularly valuable in treating biofilm-associated infections, where bacteria are shielded from traditional antibiotics. AI-driven models can predict which combinations of antibiotics, nanoparticles, or phages will be most effective in penetrating biofilms and eliminating the bacteria within.
Challenges and the Road Ahead
Regulatory and Economic Challenges
Despite the promising breakthroughs in next-generation antibiotics, significant challenges remain. One of the main obstacles is the regulatory approval process. New antibiotics must undergo rigorous testing to ensure their safety and efficacy, which can take years and require significant financial investment. This lengthy process, combined with the limited profitability of antibiotics, has deterred many pharmaceutical companies from pursuing antibiotic development.
Efforts are being made to incentivize the development of new antibiotics, including government subsidies, grants, and extended market exclusivity for successful drugs. Collaborative efforts between governments, research institutions, and private companies are essential to overcoming the economic and regulatory barriers to bringing next-generation antibiotics to market.
Ensuring Sustainable Use
The development of next-generation antibiotics is only part of the solution. Ensuring that these drugs are used responsibly is crucial to preventing the further spread of resistance. Stewardship programs aimed at reducing the overuse and misuse of antibiotics in both healthcare and agriculture are essential for preserving the effectiveness of new treatments.
Public education campaigns and stricter regulations on antibiotic use in agriculture and livestock farming can help reduce the selection pressure that drives the evolution of resistant bacteria.
Conclusion: The Future of Antibiotics
Next-generation antibiotics represent a beacon of hope in the fight against antibiotic resistance. Through novel classes of antibiotics, advancements in drug delivery systems, the revival of older treatments with innovative approaches, and the integration of AI in drug discovery, the medical community is making significant strides in combating superbugs.
However, the road to widespread availability of these breakthroughs is still fraught with challenges. Continued investment in research, regulatory reform, and global collaboration will be critical to ensuring that these innovations reach the patients who need them most. With the right support, next-generation antibiotics could play a pivotal role in safeguarding the future of healthcare.
References
- World Health Organization. “Antimicrobial Resistance.” WHO Fact Sheet, 2021, pp. 1–6.
- Liu, B., & Pop, M. (2020). Antibiotic resistance genes and human microbiomes. International Journal of Environmental Research and Public Health, 47(2), 111-120. https://doi.org/10.3390/ijerph17020447
- Tacconelli, E., Carrara, E., Savoldi, A., et al. (2018). Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. The Lancet Infectious Diseases, 18(3), 318-327. https://doi.org/10.1016/S1473-3099(17)30753-3.
- Hutchings, M. I., Truman, A. W., & Wilkinson, B. (2019). Antibiotics: past, present and future. Current Opinion in Microbiology, 51, 72-80.https://doi.org/10.1016/j.mib.2019.10.008.
- Ventola, C. L. (2015). The antibiotic resistance crisis: Causes and threats. Pharmacy and Therapeutics, 40(4), 277-283. PMCID:
- Wright, G. D. (2019). Unlocking the potential of natural products in antibiotic discovery. Nature Reviews Drug Discovery, 18(5), 267-285. https://doi.org/10.1111/1751-7915.13351.
FAQ
- What is antibiotic resistance?
Antibiotic resistance occurs when bacteria evolve to survive drugs designed to kill them. This makes infections harder to treat, leading to severe health risks. - Why is antibiotic resistance a major health threat?
Resistant infections can lead to longer hospital stays, higher medical costs, and increased mortality, with some common infections becoming nearly untreatable. - What are “superbugs”?
Superbugs are bacteria resistant to multiple antibiotics, such as MRSA and CRE. These infections are challenging to treat and often require last-resort therapies. - What are next-generation antibiotics?
Next-generation antibiotics are newly developed drugs targeting resistant bacteria. They may include novel antibiotic classes, revived older drugs, and innovative treatment methods. - How is AI helping in antibiotic development?
AI helps researchers analyze data to find new drug candidates and predict bacterial resistance, speeding up the discovery of effective antibiotics. - What role does nanotechnology play?
Nanotechnology enables targeted delivery of antibiotics, helping drugs reach infection sites more effectively and bypass bacterial defenses, such as biofilms. - What are antimicrobial peptides (AMPs)?
AMPs are naturally occurring molecules that disrupt bacterial membranes, making them effective against resistant strains and offering new treatment options. - How can I help combat antibiotic resistance?
Avoid unnecessary antibiotic use, follow prescribed treatments, and support policies that promote responsible antibiotic use in healthcare and agriculture. - Are there ways to revive older antibiotics?
Yes, combining older antibiotics with adjuvants or using structural modifications can help restore their effectiveness against resistant bacteria. - What’s the future of antibiotics?
Through global collaboration, technological innovation, and responsible use, next-generation antibiotics offer hope in managing and reducing antibiotic resistance.